The Role of Stents in Treating Prostate Problems
What is a Stent?
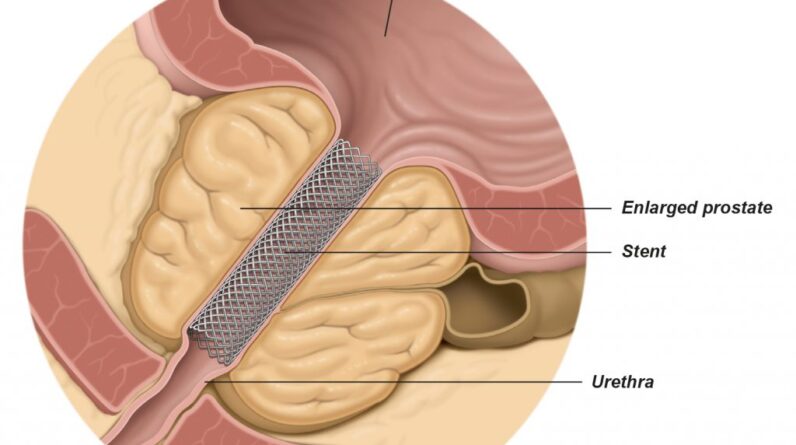
A stent is a small tube-like structure used to keep body passages open, aiding normal function.
How Stents Work
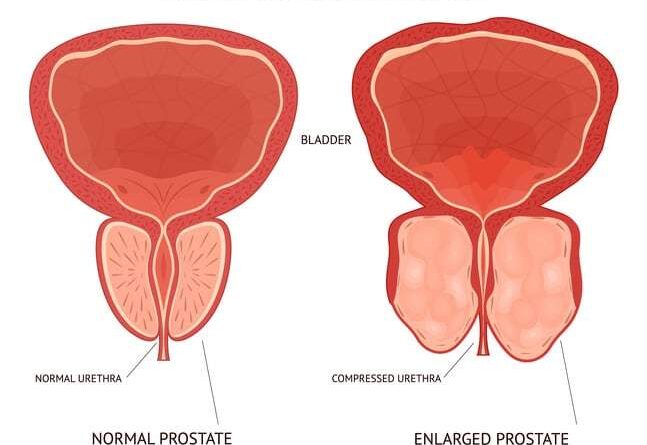
In the context of prostate issues, stents keep the urethra open, alleviating symptoms caused by a swollen prostate pressing against it.
The Use of Stents in Prostate Treatment
Stents are often used as a temporary solution or when surgery is not a viable option for patients.
Benefits of Using Stents in Prostate Treatment
The benefits include improved urinary flow, lesser pain, and a better quality of life.
Stents and Prostate Surgery
Prostate surgery, or prostatectomy, involves removing part or all of the prostate gland.
How Stents Complement Prostate Surgery
A stent can help ensure the urinary passage remains open during the healing process post-surgery.
Stents in Post-surgery Recovery
In post-surgery recovery, stents aid in reducing urinary problems and speeding up recovery.
Risks and Considerations
While stents offer relief, they come with potential risks, such as infection, dislocation, or urinary incontinence.
Making the Decision: Pros and Cons
It’s crucial to weigh the benefits and drawbacks with your healthcare provider before deciding.
Living with a Prostate Stent
Life with a stent may involve slight changes to your daily routine. It’s often advised to avoid strenuous activities, which could displace the stent. But most daily activities can be resumed.
Long-term Effects and Considerations
In the long term, some men may experience discomfort during urination. However, for most, the relief from symptoms often outweighs the potential discomfort.
Recap and Final Thoughts
Now that we’ve delved into the world of prostate problems and the role of stents, it’s clear that while this approach isn’t without its drawbacks, it can be a life-altering solution for many. The key is understanding your own body, working closely with your medical professional, and weighing all available options.
In Conclusion
Ultimately, dealing with prostate problems can be challenging, but there are options, like the use of stents, that can greatly help. Make sure you have open and honest conversations with your doctor to choose the best course of action.
FAQs
1. Can a stent cure prostate problems permanently?
No, stents are typically a temporary solution or used for those who cannot undergo surgery.
2. Are there alternatives to stents for treating prostate problems?
Yes, options can range from medication to different types of surgeries, like transurethral resection of the prostate (TURP).
3. Are stents painful?
Most patients report slight discomfort rather than pain, and this usually subsides after some time.
4. Can I live a normal life with a stent?
Most people can continue with their daily activities, albeit with slight modifications.
5. How long does a stent last in the prostate? Stents can stay for a few weeks to a few months, depending on the type and patient’s condition. Your doctor will provide specific guidance.
6. Can a stent be removed once it’s placed?
Yes, stents are designed to be removed or replaced as needed under the guidance of a healthcare professional.
7. Are there any dietary restrictions while living with a prostate stent?
While there aren’t specific dietary restrictions, maintaining a healthy diet and staying hydrated can help your body function optimally and potentially alleviate some symptoms related to prostate problems.
8. Can a prostate stent help with prostate cancer?
Stents can relieve symptoms associated with prostate cancer, such as urinary problems, but they do not treat the cancer itself.
9. What’s the success rate of using stents for prostate problems?
The success rate varies based on individual circumstances, including the nature and severity of the prostate problem. It’s best to discuss this with your healthcare provider for personalized information.
10. Is the stent insertion procedure painful? The procedure is typically performed under anesthesia, so patients should not feel pain during insertion. Post-procedure, there may be some discomfort which usually subsides over time.